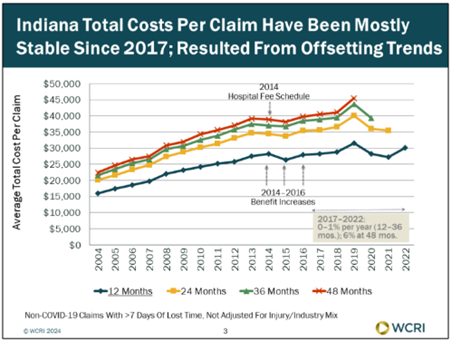
Worker’s compensation costs per claim largely stable since 2017
Indemnity benefits per workers’ compensation claim grew at a rapid pace of six percent or more in 2022 in 16 out of 17 study states, with eight states growing at a rate of 10% or more, but Indiana increasing by only 3.0% – below the 4.0% median state rate – according to a new set of studies from the Workers Compensation Research Institute (WCRI). This followed a period of little change overall in most study states from 2019 to 2021. In 2022, the average medical payment per claim in Indiana increased 12%, driven by payments greater than $50,000.
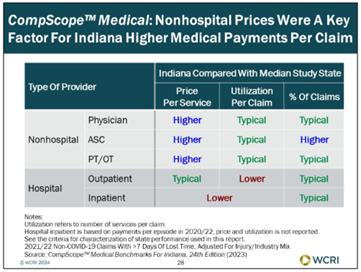
At an average of $41,122, total costs per claim with more than seven days of lost time in Indiana were in the middle of the study states for 2020 claims with an average of 36 months of experience. While medical payments per claim were higher than typical of the study states, indemnity benefits per claim and benefit delivery expenses per claim in Indiana were lower than typical. Higher payments for nonhospital services (mainly higher prices) were the principal reason for the higher medical payments per claim, according to WCRI . . . which notes that utilization of nonhospital care was mostly typical in Indiana.
Nonhospital care costs related to physicians, ambulatory surgery centers (ASCs) and physical and occupational therapy were generally higher than in other states, while hospital-related expenses – inpatient and outpatient – were invariably the same or lower than in other states. Indiana does, however, register a higher-than-typical percentage of claims with facility services, likely related to a higher surgery rate, the researchers note.
Total costs per claim were mostly stable in Indiana during the 2017 – 2022 study period, although large year-to-year fluctuations were found, with different underlying factors contributing to the result in each year. For example, WCRI researchers believe that changes in the mix of claims and their medical severity likely resulted in large increases in medical payments greater than $100,000 during some years; pandemic-related factors led to decreases in medical utilization; and resumption of economic activity in 2021–2022 likely contributed to changes in the mix of claims, leading to high-cost medical payments, increases in workers’ wages, and duration of temporary disability (since the beginning of the pandemic, increases in duration of temporary disability in Indiana have been smaller than in most other study states).
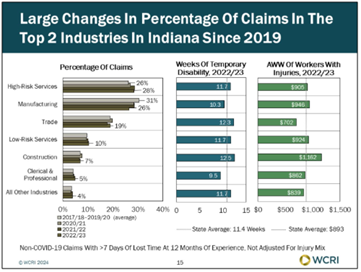
During 2022, the growth in the average weekly wage (AWW) of workers with job-related injuries accelerated by seven percent in Indiana compared with three percent per year in the prior two years; AWW grew at faster-than-typical rates in many industries in Indiana, and it increased for all job tenure categories in the Hoosier State. Indiana also sees the average duration of temporary disability increase by 0.6 weeks in 2022, following small changes in the prior two years.
Between 2014 and 2016, WCRI researchers find that a combination of offsetting changes affected total costs per claim. A statutory increase in income benefits from 2014 to 2016 led to a 14% increase in indemnity benefits per claim during that period, while the introduction of the hospital fee schedule in 2014 led to a one-time decrease of 11% in medical payments per claim. Changes in total costs per claim after 2018 were driven by medical payments.
The WCRI team also documents large changes in the percentage of claims in the largest industries in Indiana, with most of these changes occurring during the pandemic. The claim share of high-risk services increased from about 26% (2017 – 2019) to 28% in 2022. In contrast, the claim share in manufacturing decreased from 31% to 26%; and the claim share in trade fluctuated (18% – 20%). These three industries combined accounted for almost three-quarters (73%) of all claims in 2022.